Coronary Artery Bypass Surgery(CABG)
BYPASS SURGERY
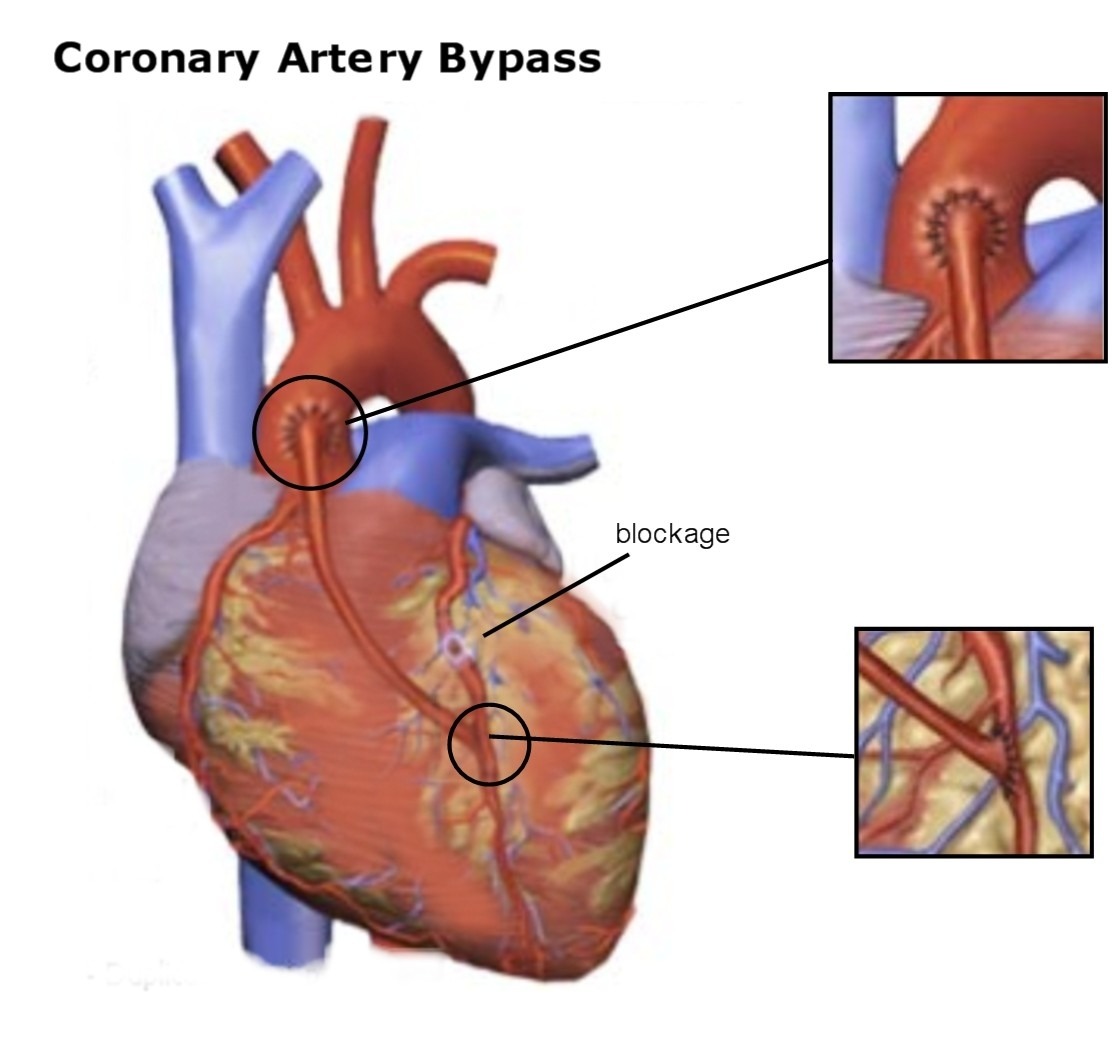
Bypass surgery is the most common type of heart surgery. Arteries can become clogged over time by the buildup of fatty plaque. Bypass surgery improves the blood flow to the heart with a new route, or “bypass,” around a section of clogged or diseased artery.
The surgery involves sewing a section of vein from the leg or artery from the chest or another part of the body to bypass a part of the diseased coronary artery. This creates a new route for blood to flow, so that the heart muscle will get the oxygen-rich blood it needs to work properly.
During bypass surgery, the breastbone (sternum) is divided; the heart may or may not be stopped. Beating heart surgery is very common now and blood is sent through a heart-lung machine only if the heart is stopped. Unlike other forms of heart surgery, the chambers of the heart are not opened during the operation.
WHAT HAPPENS DURING CABG?
Your Cardiologist after evaluation of your reports of al tests carried out after you had reported to him will advise you about the next course of treatment. Angiography would have probably already been conducted. An angiogram reveals the location of the blockage and its extent for each vessel of the tested area. The doctor after study of the findings will explain to you or your relatives about the results and future course of action for you. He may opt for any of the following:
- In case the blockages are minimal- below 50% you may be advised to carry on taking prescribed medicines and periodic evaluation along with necessary precautionary measures.
- You may have blockages in 1 or 2 arteries and the size of the same may also be reasonably small. In this case you will be advised to undergo ANGIOPLASTY with or without stenting.
- In the event of your having multiple blockages or very long lesions in 1 or more arteries which cannot be treated with Angioplasty, you will be advised to undergo Coronary Bypass Grafting Surgery (CABG).
The operation will usually be scheduled at a time that is best for you and your surgeon, except in urgent cases. In your interest you should try and schedule the surgery at the earliest to avoid further damage to the heart muscle. As the date of your surgery gets closer, be sure to tell your surgeon and cardiologist about any changes in your health. If you have a cold or the flu, this can lead to infections that may affect your recovery. Be aware of fever, chills, coughing, or a runny nose. Tell the doctor if you have any of these symptoms.
Also, remind your cardiologist and surgeon about all of the medicines you are taking, especially any over-the-counter medicines such as aspirin or those that might contain aspirin. You should make a list of the medicines and bring it with you to the hospital.
It is always best to get complete instructions from your cardiologist and surgeon about the procedure, but here are some basics you can expect as a bypass patient.
BEFORE HOSIPTALISATION
Before coming to the hospital for surgery you must consult your surgeon about stopping the use of certain type of medicines a day or two before surgery. The Cardiologist would have prescribed anti-clotting medicines to you as part of your treatment. These are stopped before surgery.
Most patients are admitted to the hospital a day before surgery or, in some cases, on the morning of surgery.
The night before surgery, you will be asked to bathe to reduce the amount of germs on your skin. After you are admitted to the hospital, the area to be operated on will be washed, scrubbed with antiseptic, and, if needed, shaved.
A medicine (anesthetic) will be given to make you sleep during the operation. This is called “anesthesia.” Because anesthesia is safest on an empty stomach, you will be asked not to eat or drink after midnight the night before surgery. If you do eat or drink anything after midnight, it is important that you tell your anesthesiologist and surgeon.
If you smoke, your doctor will want you to stop at least 2 weeks before your surgery. Smoking before surgery can lead to problems with blood clotting and breathing.
Your Surgeon will invariably brief you and your close relatives about following aspects of CABG:
- The procedure itself, approximate time etc.
- Risk factors
- Total risk to life- in a normal patient with reasonable good condition of the heart this risk is placed at around 2-3%.
- Your consent for the surgery and you will be required to sign the consent papers.
- Any special instructions.
You should clarify all doubts at this stage to make an informed decision.
ON THE DAY OF SURGERY
Before surgery, you may have to have an Electrocardiogram (ECG), blood tests, urine tests, and a chest x-ray to give your surgeon the latest information about your health. You will be given something to help you relax (a mild tranquilizer) before you are taken into the operating room.
Small metal disks called electrodes will be attached to your chest. These electrodes are connected to an electrocardiogram machine, which will monitor your heart’s rhythm and electrical activity.
Before you are taken to the Operation Theatre you will be allowed to meet your spouse or other relatives present in the hospital at that time.
INSIDE THE OPERATION THEATRE
You will receive a local anesthetic to numb the area where a plastic tube (called a line) will be inserted in an artery in your wrist. An intravenous (IV) line will be inserted in your vein / artery in the neck. The IV line will give you the anesthesia during the operation.
After you are completely asleep, a tube will be inserted down your windpipe and connected to a machine called a respirator, which will take over your breathing. Another tube will be inserted through your nose and down your throat, into your stomach. This tube will stop liquid and air from collecting in your stomach, so you will not feel sick and bloated when you wake up. A thin tube called a catheter will be inserted into your bladder to collect any urine produced during the operation.
The surgeon will decide the mode of surgery on your physiological condition. He may opt for Beating Heart surgery Or Stop your heart during surgery.
The cardiac surgeon makes an incision down the middle of the chest and then saws through the breastbone (sternum). This procedure is called a median (middle) sternotomy (cutting of the sternum).
The heart is cooled with iced salt water, while a preservative solution is injected into the heart arteries. This process minimizes damage caused by reduced blood flow during surgery and is referred to as “cardioplegia.” Before bypass surgery can take place, a cardiopulmonary bypass must be established. Plastic tubes are placed in the right atrium to channel venous blood out of the body for passage through a plastic sheeting (membrane oxygenator) in the heart-lung machine. The oxygenated blood is then returned to the body. The main aorta is clamped off (cross-clamped) during CABG surgery to maintain a bloodless field and to allow bypasses to be connected to the aorta.
The most commonly used vessel for the bypass is the saphenous vein from the leg. Bypass grafting involves sewing the graft vessels to the coronary arteries beyond the narrowing or blockage. The other end of this vein is attached to the aorta. Chest wall arteries, particularly the left internal mammary artery, have been increasingly used as bypass grafts. This artery is separated from the chest wall and usually connected to the left anterior descending artery and/or one of its major branches beyond the blockage. The major advantage of using internal mammary arteries is that they tend to remain open longer than venous grafts. Ten years after CABG surgery, only 66% of vein grafts are open compared to 90% of internal mammary arteries. However, artery grafts are of limited length, and can only be used to bypass diseases located near the beginning (proximal) of the coronary arteries. Using internal mammary arteries may prolong CABG surgery because of the extra time needed to separate them from the chest wall. Therefore, internal mammary arteries may not be used for emergency CABG surgery when time is critical to restore coronary artery blood flow.
CABG surgery takes about four hours to complete. The aorta is clamped off for about 60 minutes and the body is supported by cardiopulmonary bypass for about 90 minutes. The use of 3 (triple), 4 (quadruple), or 5 (quintuple) bypasses are now routine. At the end of surgery, the sternum is wired together with stainless steel and the chest incision is sewn closed. Plastic tubes (chest tubes) are left in place to allow drainage of any remaining blood from the space around the heart (mediastinum).
About 5% of patients require exploration within the first 24 hours because of continued bleeding after surgery. Chest tubes are usually removed the day after surgery. The breathing tube is usually removed shortly after surgery. Patients usually get out of bed and are transferred out of intensive care a day or two after surgery. Up to 25% of patients develop heart rhythm disturbances within the first three or four days after CABG surgery. These rhythm disturbances are usually temporary atrial fibrillation and are felt to be related to surgical trauma to the heart. Most of these arrhythmias respond to standard medical therapy that can be weaned one month after surgery. The average length of stay in the hospital for CABG surgery has been reduced from as long as a week to only three to four days in most patients. Many young patients can even be discharged home after two days.
A new advance for many patients is the ability to do CABG without going on cardiopulmonary bypass (“off-pump”), with the heart still beating. This significantly minimizes the occasional memory defects and other complications that may be seen after CABG, and is a significant advance.
HOW LONG WILL I TAKE TO RECOVER AFTER CABG?
Sutures are removed from the chest prior to discharge and from the leg (if the saphenous vein is used) after 7 to 10 days. Even though smaller leg veins will take over the role of the saphenous vein, a certain degree of swelling in the affected ankle is common. Patients are advised to wear elastic support stockings during the day for the first four to six weeks after surgery and to keep their leg elevated when sitting. This swelling usually resolves after about six to eight weeks.
Healing of the breastbone takes about six weeks and is the primary limitation in recovering from CABG surgery. Patients are advised not to lift anything more than 10 pounds or perform heavy exertion during this healing period. They are also advised not to drive for the first four weeks to avoid any injury to the chest. Patients can return to normal sexual activity as long as they minimize positions that put significant weight on the chest or upper arms. Return to work usually occurs after the six week recovery, but may be much sooner for non–strenuous employment.
Exercise stress testing is routinely done four to six weeks after CABG surgery and signals the beginning of a cardiac rehabilitation program. Rehabilitation consists of a 12 week program of gradually increasing monitored exercise lasting one hour three times a week.
Patients are also counseled about the importance of lifestyle changes to lower their chance of developing further CAD. These include STOPPING SMOKING, reducing weight and dietary fat, controlling blood pressure and diabetes, and lowering blood cholesterol levels.
WHAT RESTRICTIONS ARE PLACED AFTER CABG?
Post CABG a patient is required to strictly follow the instructions of the surgeon. You may be called for a check-up about 1 week after your discharge from the hospital. Thereafter, the visits may be scheduled once a month or after a longer period/ on occurrence of any discomfort.
After bypass surgery, you should limit the fat and cholesterol in your diet. Your doctor may recommend walking or swimming to get your strength back. Your doctor may also recommend that you join a cardiac rehabilitation program. These programs can help you make lifestyle changes such as starting a new diet and exercise program, quitting smoking, and learning to better deal with stress.
If you have an office job, you can usually go back to work in 4 to 6 weeks. Those who have more physically demanding jobs may need to wait longer. In some extreme cases, you may need to find a job that is not as physically demanding. Twenty to 30% of bypass patients will need a second procedure within 10 years.
WHAT ARE THE RISKS OF CABG SURGERY?
Overall mortality related to CABG is 3–4%. During and shortly after CABG surgery, heart attacks occur in 5 to 10% of patients and are the main cause of death. About 5% of patients require exploration because of bleeding. This second surgery increases the risk of chest infection and lung complications. Stroke occurs in 1–2%, primarily in elderly patients. Mortality and complications increase with:
- age (older than 70 years),
- poor heart muscle function,
- disease obstructing the left main coronary artery,
- diabetes,
- chronic lung disease,
- chronic kidney failure.
Mortality may be higher in women, primarily due to their advanced age at the time of CABG surgery and smaller coronary arteries. Women develop coronary artery disease about 10 years later than men because of hormonal “protection” while they still regularly menstruate (although in women with risk factors for coronary artery disease, especially smoking, elevated lipids, and diabetes, the possibility for the development of coronary artery disease at a young age is very real). Women are generally of smaller stature than men, with smaller coronary arteries. These small arteries make CABG surgery technically more difficult and prolonged. The smaller vessels also decrease both short and long–term graft function.
LONG TERM EFFECTS / RESULTS OF CABG SURGERY?
A very small percentage of vein grafts may become blocked within the first two weeks after CABG surgery due to blood clotting. Blood clots form in the grafts usually because of small arteries beyond the insertion site of the graft causing sluggish blood run off.
Another 10% of vein grafts close off between two weeks and one year after CABG surgery. Use of aspirin to thin the blood has been shown to reduce these later closings by 50%.
Grafts become narrowed after the first five years as cells stick to the inner lining and multiply, causing formation of scar tissue (intimal fibrosis) and actual atherosclerosis.
After 10 years, only 2/3 of vein grafts are open and 1/2 of these have at least moderate narrowing’s. Internal mammary grafts have a much higher (90%) 10 year rate of remaining open. This difference in longevity has caused a shift in surgical practices toward greater use of internal mammary and other arteries as opposed to veins for bypasses.
Recent data has shown that in CABG patients with elevated LDL cholesterol (bad cholesterol) levels, use of cholesterol-lowering medications (STATINS) to lower LDL levels to below 80 will significantly improve long–term graft patency as well as improve survival benefit and heart attack risk.
Patients are also advised about the importance of lifestyle changes to lower their chance of developing further atherosclerosis in their coronary arteries. These include stopping smoking, exercise, reducing weight and dietary fat, as well as controlling blood pressure and diabetes.
Frequent monitoring of CABG patients with physiologic testing can identify early problems in grafts. PTCA (angioplasty) with stenting, in addition to aggressive risk factor modification, may significantly limit the need for repeat CABG years later. Repeat CABG surgery is occasionally necessary, but may have a higher risk of complication.
CABG SURGERY OR ANGIOPLASTY (PTCA) – WHICH IS BETTER?
Ongoing studies are comparing the treatment results of angioplasty (PTCA) versus bypass (CABG surgery) in patients who are candidates for either procedure.
Both procedures are very effective in reducing angina symptoms, preventing heart attacks, and reducing death. Many studies have either shown similar benefits or slight advantage to CABG (primarily in severe diabetics), although current studies are evaluating the two procedures utilizing the most current improved techniques (for example, newer “medicated” stents and the off–pump CABG); this data is still being collected.
The best choice for an individual patient is best made by their cardiologist, surgeon, and primary doctor
Facebook Comments